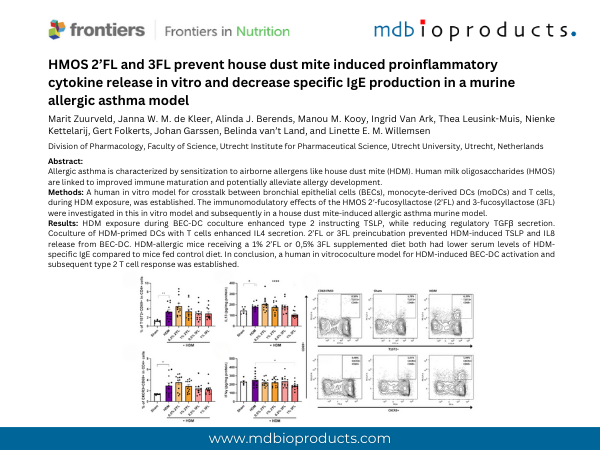
Featured Publication in Focus: HMOS 2’FL and 3FL prevent house dust mite induced proinflammatory cytokine release in vitro and decrease specific IgE production in a murine allergic asthma model
Apr 23 , 2025
Authors:
Marit Zuurveld, Janna W. M. de Kleer, Alinda J. Berends, Manou M. Kooy, Ingrid Van Ark, Thea Leusink-Muis, Nienke Kettelarij, Gert Folkerts, Johan Garssen, Belinda van’t Land, and Linette E. M. Willemsen
Division of Pharmacology, Faculty of Science, Utrecht Institute for Pharmaceutical Science, Utrecht University, Utrecht, Netherlands
Frontiers in Nutrition. Nutritional Immunology
----------------------
Product referenced:
Catalogue # 101001F
Rat Monoclonal Antibody to Mouse T1/ST2 FITC Conjugated
----------------------
ABSTRACT
Introduction: Allergic asthma is characterized by sensitization to airborne allergens like house dust mite (HDM). Human milk oligosaccharides (HMOS) are linked to improved immune maturation and potentially alleviate allergy development.
Methods: A human in vitro model for crosstalk between bronchial epithelial cells (BECs), monocyte-derived DCs (moDCs) and T cells, during HDM exposure, was established. The immunomodulatory effects of the HMOS 2′-fucosyllactose (2’FL) and 3-fucosyllactose (3FL) were investigated in this in vitro model and subsequently in a house dust mite-induced allergic asthma murine model.
Results: HDM exposure during BEC-DC coculture enhanced type 2 instructing TSLP, while reducing regulatory TGFβ secretion. Coculture of HDM-primed DCs with T cells enhanced IL4 secretion. 2’FL or 3FL preincubation prevented HDM-induced TSLP and IL8 release from BEC-DC. HDM-allergic mice receiving a 1% 2’FL or 0,5% 3FL supplemented diet both had lower serum levels of HDM- specific IgE compared to mice fed control diet. In conclusion, a human in vitrococulture model for HDM-induced BEC-DC activation and subsequent type 2 T cell response was established. 2’FL or 3FL preincubation of BEC-DC prevented HDM-induced activation and modified downstream T cell responses in vitro. Both HMOS reduced HDM-specific IgE in a murine model for HDM allergic asthma, but did not protect against airway inflammation.
Conclusion: Here, we describe an in vitro human airway mucosal HDM sensitization model as relevant tool to reduce use of animals in studies aiming to prevent HDM allergic asthma. Both in vitro as well as in vivo, HMOS were found to drive away from a type 2 immune signature, paving the way to further investigate the potential allergy preventive effects of fucosylated HMOS.
To continue reading and to download the publication:
https://doi.org/10.3389/fnut.2025.1491430